The application of hypnosis in medical and psychological contexts has a history stretching back several centuries. In the 18th century, Austrian physician Franz Anton Mesmer proposed that “mesmerism” was caused by an unseen fluid flowing between the healer and the patient. Over time, this concept was replaced by more scientific explanations, but the therapeutic potential of hypnosis persisted, especially for individuals with mental health challenges and those undergoing surgical procedures.
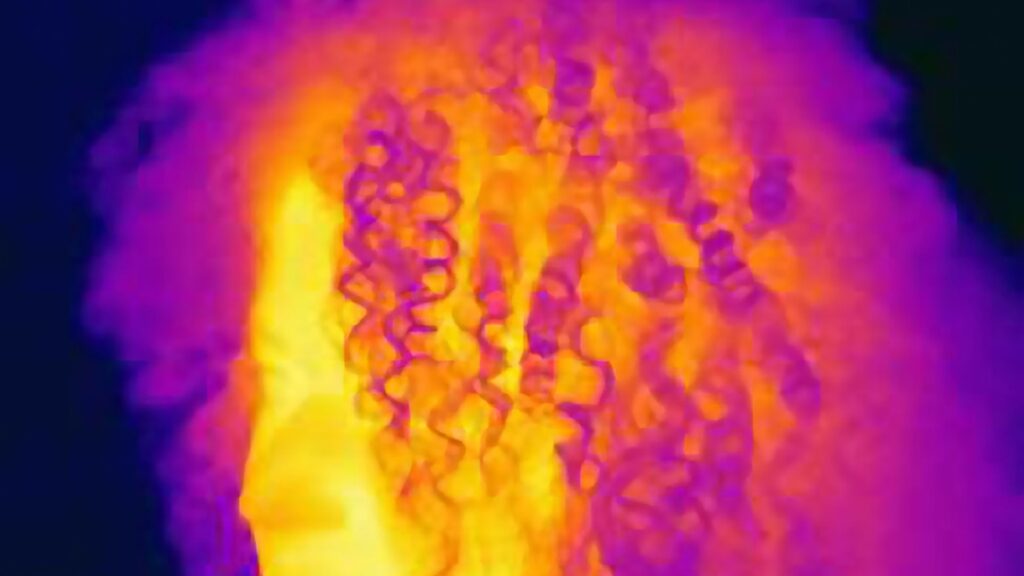
Today, hypnosis is recognized as a mental state characterized by heightened suggestibility, where perceptions and memories can be influenced through targeted suggestions. Although our understanding of hypnotic states has advanced significantly, the technique remains a valuable adjunct in both clinical psychology and medicine. Modern applications include managing addiction, alleviating chronic pain, and more recently, reducing hot flashes associated with menopause.
Menopause typically occurs between ages 45 and 55, marked by a decline in estrogen and progesterone production, leading to the cessation of menstruation. This hormonal shift often triggers hot flashes-sudden feelings of intense heat, sweating, anxiety, and chills-that can significantly impair quality of life. (Discover more about the physiological changes during menopause)
Some experts suggest that hypnosis could serve as an alternative or complementary approach to hormone therapy, which can be costly and carry potential risks. Although it might seem unconventional, there is growing evidence supporting the use of hypnotic techniques to manage menopausal symptoms. A comprehensive review conducted by researchers at Baylor University in 2025 found that, compared to cognitive behavioral therapy (CBT), hypnosis was more effective in decreasing both the frequency and severity of hot flashes.
Let’s explore the scientific basis behind hypnosis for hot flash relief-what it involves and how it might genuinely influence the body’s response to menopausal symptoms.
(Is this hypnotic health trend a genuine breakthrough or just a placebo illusion?)
Understanding the Origins and Treatments of Hot Flashes
To effectively address hot flashes, it’s essential to understand their root causes. According to Gary Elkins, a clinical psychologist and lead author of recent research reviews at Baylor University, “It’s not solely the drop in estrogen that triggers hot flashes.”
During menopause, the hypothalamus-the brain’s temperature regulation center-misinterprets hormonal fluctuations as signals of overheating. This misperception results in the body initiating cooling responses, such as sweating and vasodilation, to lower perceived internal temperature. Elkins explains, “The hormonal shifts during menopause cause the hypothalamus to perceive heat, leading to the characteristic hot flashes.”
Common treatments include hormone replacement therapy (HRT), which restores hormone levels, and non-hormonal options like Veozah (fezolinetant), gabapentin, and clonidine, which target neural pathways involved in temperature regulation. The North American Menopause Society also endorses cognitive behavioral therapy (CBT) as an effective non-hormonal intervention.
How Hypnosis May Influence Hot Flash Triggers
Elkins and his team analyzed numerous studies on hot flashes and behavioral interventions. Their review of 23 clinical trials revealed that after just one week of hypnotic treatment, women experienced an average reduction of approximately 30% in hot flash frequency. By the fourth week, this reduction increased to around 70%. In contrast, CBT showed less pronounced effects in similar studies.
What could be happening within the brain to produce such results? Elkins hypothesizes that during hypnosis, post-hypnotic suggestions may alter the hypothalamus’s perception of temperature, effectively reducing the body’s heat signals and the occurrence of hot flashes.
Additionally, stress and anxiety are significant triggers for hot flashes. Hypnotic relaxation techniques can help women manage these emotional responses, leading to a decrease in hot flash episodes even outside of the hypnotic state. This suggests that hypnosis may influence the autonomic nervous system, which governs involuntary bodily functions.
Elkins emphasizes that consistent practice is crucial. “You can’t expect a single hypnosis session to eliminate hot flashes entirely. It’s about reinforcing the mind-body connection through ongoing practice and suggestion,” he notes.
What Does Hypnosis for Hot Flashes Look Like?
Mary Cahilly, a licensed mental health therapist specializing in holistic wellness, incorporates hypnosis into her treatment options at Canyon Ranch, a renowned health resort in Lenox, Massachusetts. Her approach often begins with guiding clients to recall a deeply pleasant memory, which promotes relaxation. “When we evoke a positive memory, the limbic system in the brain relaxes because it cannot distinguish between imagination and reality,” Cahilly explains. This relaxation state then facilitates the hypnotic trance.
For hot flashes, Cahilly describes the hypnotic experience as a sensation of being in tune with one’s body-feeling cool, light, and free from discomfort. A key component is the use of post-hypnotic suggestions, which empower women to access this relaxed state during a hot flash, helping to diminish its intensity and duration.
Hypnosis as a Safe Alternative to Conventional Medications
Many pharmaceutical options for hot flash relief come with undesirable side effects, such as dry mouth, gastrointestinal upset, drowsiness, or even more serious concerns like elevated liver enzymes. Since hypnosis does not influence estrogen levels, it sidesteps these adverse effects, making it an attractive option for many women.
While estrogen levels remain permanently reduced after menopause, the hypothalamus can recalibrate its temperature regulation over time. Elkins suggests that hypnosis might accelerate this natural adjustment process by modulating neural pathways involved in temperature perception.
Cost and accessibility are also important considerations. For example, Veozah costs approximately $550 per month, whereas hypnosis sessions-either in person or via digital platforms-are often more affordable. Online programs and apps like HypnoBox or EverCalm offer guided hypnosis sessions that women can use at home, with in-person therapy costing upwards of $250 per session but often available as recorded sessions for repeated use.
Debunking Myths: Is Hypnosis Just Wishful Thinking?
Elkins recognizes the historical skepticism surrounding women’s health issues and the tendency for their symptoms to be dismissed or misunderstood. His research indicates that the effectiveness of hypnosis does not depend on a woman’s belief or confidence in the technique. “Whether or not you believe in hypnosis, the results can still be significant,” he states.
While hypnosis shares similarities with mindfulness and relaxation techniques, studies show that these practices alone do not significantly reduce hot flashes. Neither mindfulness nor relaxation exercises have demonstrated a consistent impact on the frequency or severity of symptoms, unlike hypnosis.
Is Hypnosis a Placebo Effect?
Some experts argue that the benefits of hypnosis may largely stem from placebo effects-the power of the mind to influence bodily processes through expectation and suggestion. Michael Lifshitz, an assistant professor at McGill University, notes, “Hypnosis might be considered an extraordinary placebo, where the mind’s influence on the body is harnessed to produce real physiological changes.”
However, Lifshitz clarifies that placebo is not merely wishful thinking. “Placebo effects are genuine; they can alter bodily functions in tangible ways,” he explains. Ted Kaptchuk, a Harvard Medical School professor, emphasizes that placebos work by modulating symptoms, not by curing underlying diseases. “In the case of hot flashes, the brain’s response to suggestion can diminish the nerve signals that trigger these episodes,” he says.
In a 2020 study, Kaptchuk explored the effects of open-label placebos-where patients are aware they are not taking active medication-and found that even this transparency can lead to symptom improvement. This suggests that the mind’s expectation and attention can significantly influence physical experiences.
While the placebo component may contribute to hypnosis’s effectiveness, Elkins points out that the primary goal is symptom relief. “If women see that hypnosis reduces their hot flashes, they often don’t care whether it’s a placebo or not,” he remarks.